
Hello, you are using an old browser that's unsafe and no longer supported. Please consider updating your browser to a newer version, or downloading a modern browser.
Hello, you are using an old browser that's unsafe and no longer supported. Please consider updating your browser to a newer version, or downloading a modern browser.
Breastfeeding can be a wonderful experience, but it can also be a challenge at times. We hope these resources are helpful to you as you establish your breastfeeding journey. If there’s a topic you think we missed – reach out to us!
Some ways you can tell if your baby has a good latch are:

Source: Office on Women’s Health
If you have any questions about your breast pump and/or flange size, please reach out to a lactation consultant. They can be very helpful! (4)
If your sore/cracked nipples are not improving after treating at home, or if you notice possible symptoms of an infection (warmth, swelling, redness, etc), it might be time to reach out to your healthcare provider. (8)
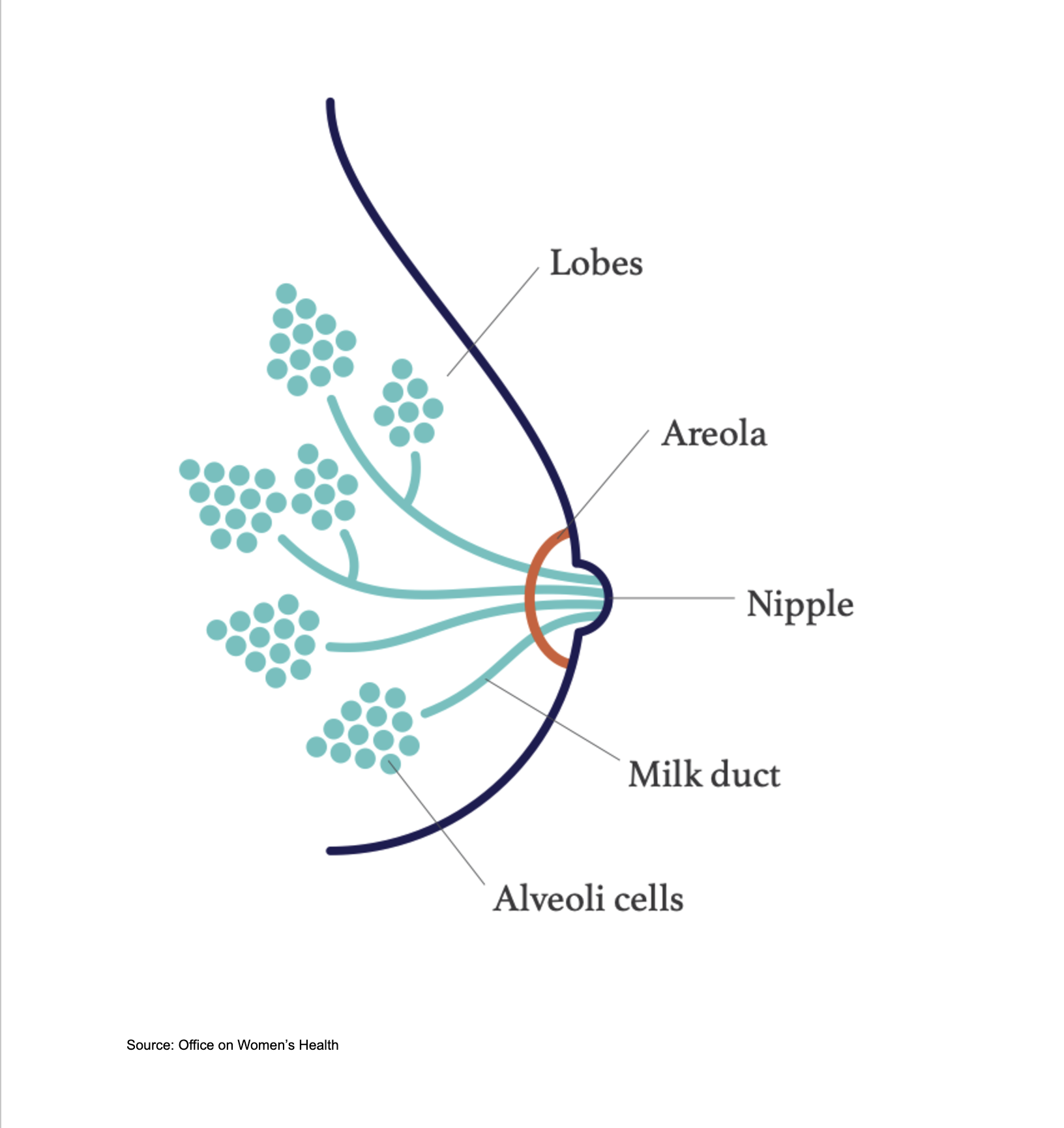
Image Source: Office on Women’s Health