1998
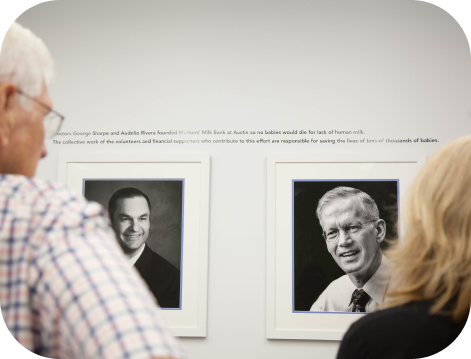
Two Austin neonatologists, Dr. Sonny Rivera and Dr. George Sharpe, invited other healthcare providers to discuss the formation of a milk bank to serve the Central Texas region. Drs. Sharpe and Rivera had observed that the tiny preterm and ill babies in the neonatal intensive care units (NICUs) they supervised fared better on human milk. Citing the medical literature that documented better health outcomes and lower care costs for infants receiving mothers’ milk – and noting that the nearest milk bank was in Denver – the two physicians gathered support from their hospitals and colleagues to go ahead with the project. An advisory board was created and a name was chosen: Mothers’ Milk Bank at Austin.
2000
After just one year of operation, we'd nearly eradicated necrotizing enterocolitis (NEC) from Austin hospitals, reducing the rate of NEC among premature births from 9% to 1% across the city. With proven success, we expanded our scope beyond Austin city limits.
2004
Responding to a need to understand variations in preterm infant growth rates, we presented our 3-year work to document variations in fats and proteins in expressed milk from different donors using a full-spectrum spectrograph calibrated in-house to read human macronutrients. Target Pooling was created by us - a method of pooling specific volumes of milk from specific moms together to achieve a targeted nutrient-rich pool of milk.
2006
We mentored a group in Fort Worth to open a new milk bank. Modeled after MMBA, the Mothers’ Milk Bank of North Texas shared the burden of feeding all NICU babies in Texas.
2008
Dr. Sonny Rivera presented a model for calculating the need for donor human milk across the US at HMBANA's annual conference.
2009
Our 10th anniversary marked the year we served 45 hospital NICUs in Texas and several other states.
2010
We moved into our third leased location in order to expand milk processing capabilities.
2016
We purchased our own building and began construction on what would become a 15,000 sq ft community-based milk bank complete with community meeting space, walk-in freezers, and a first rate research lab.
2017
We moved into our own building, a move that dramatically increased our capacity and visibility. This expansion was possible through a significant grant from the St. David’s Foundation and other funders.
2019
We now provide milk to more than 150 hospitals in 24 states and 100 babies in communities. We've become a consultant to the international community, helping other countries develop their own milk banks, facilitating greater survival of the preterm and otherwise fragile babies.
2020
In the year of COVID-19, we responded to fears of breast milk and donor human milk by helping fund research that proved that breast milk cannot transmit the virus, and if contaminated, the virus in expressed breast milk is destroyed by Holder Pasteurization.